Early Signs of Dementia in Women
“Memory is the treasure house of the mind wherein the monuments thereof are kept and preserved”. Thomas Fuller
Early signs of dementia in women:
Early: This refers to the beginning stages or the initial phase of something. In the context of “early signs of dementia,” it means recognizing symptoms at an early stage before they become more severe or noticeable.
Signs: Signs are indications or signals that suggest something is happening or present. In this case, “early signs” of dementia are the first noticeable changes or behaviors that may indicate the presence of dementia.
Dementia: Dementia is a general term used to describe a decline in cognitive function (thinking, memory, and reasoning) severe enough to interfere with daily life. It is not a specific disease but rather a set of symptoms associated with various underlying causes.
Introduction
You may have heard that more women than men show early signs of dementia, but let’s set the record straight. Recent studies suggest there’s not enough evidence to support this claim. So, if you’re a woman, don’t fret – your risk of dementia isn’t higher just because of your gender (Beam et al., 2018).
Understanding early signs of dementia in women isn’t easy. Dementia affects everyone differently, no matter their gender, but let’s try to develop our understanding of it!
The Facts:
Let’s start by looking at what recent studies tell us about dementia and its risk factors.
According to Neergaard et al. (2016), there are certain things we can’t change (non-modifiable risk factors), like getting older and genetics that might make us more likely to develop dementia.
There are other things we can change (modifiable risk factors), like how much we exercise, nutrition, chronic stress, sleep, and whether we smoke that play a big role in whether or not we begin experiencing early signs of dementia. Norton et al. (2014) found that things like not exercising enough and smoking could make us more likely to get dementia.
Surprisingly, Neergaard et al. (2016) discovered that being a bit overweight when we’re older might not matter as much as we thought! Being obese doesn’t seem to make much of a difference according to the evidence. So, it’s not just about being thin or fat – it’s more complicated than that!

Sex Differences in Early Symptoms:
Now, let’s talk about the early signs of dementia and whether they’re different for women and men.
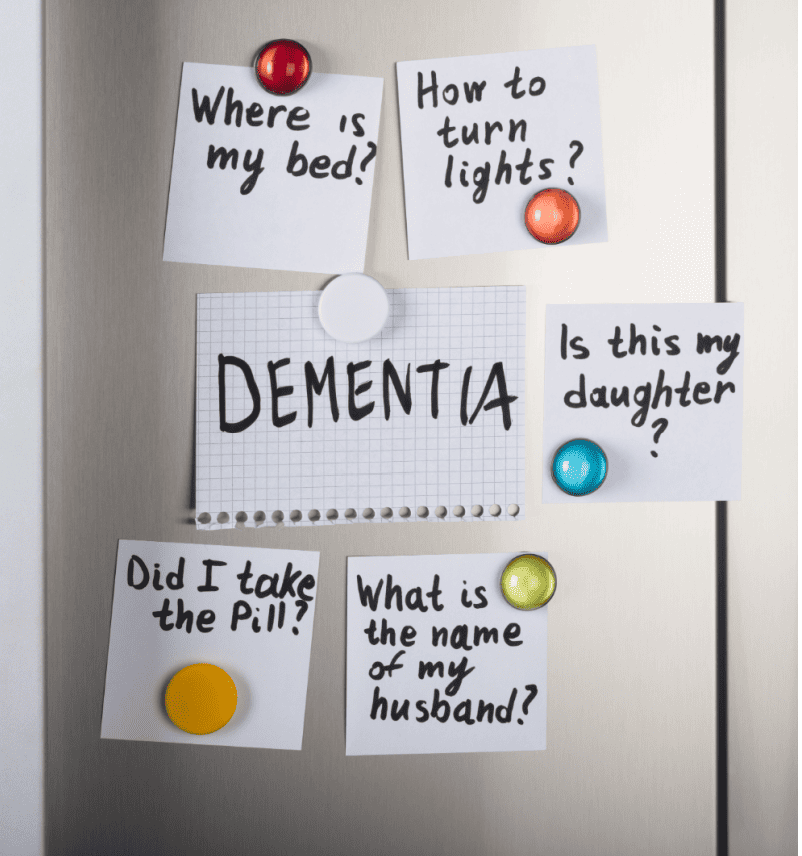
In a study by Edahiro et al. (2023), they found that women with early-onset dementia were more likely to have trouble with their memory. Men, on the other hand, were more likely to feel irritable.
Mendez (2012) also discovered that the first signs of dementia might not always be about forgetting things. Sometimes, they can be about having trouble with things like seeing things around us and paying attention.
The most common symptoms of early-onset dementia across gender are as follows:
-
- Loss of memory (Edahiro et al., 2023)
- Difficulty in word generation (Edahiro et al., 2023)
- Loss of motivation (Edahiro et al., 2023)
- Increased mistakes in the workplace or domestically (Edahiro et al., 2023)
- Unusual behaviors or attitudes (Edahiro et al., 2023)
- Visuo-spatial dysfunction (Mendez, 2012)
- Executive dysfunction (Mendez, 2012)
- Attention impairment (Mendez, 2012)
What can you do?
Stay physically active: Engage in regular physical activity, such as walking, swimming, or dancing, to promote brain health and reduce the risk of dementia
Manage depression: Seek support and treatment for depression if needed, as depression has been identified as a potential risk factor for dementia
Stay mentally active: Keep your brain stimulated by engaging in activities that challenge your cognitive abilities, such as puzzles, reading, learning new skills, or socializing with others
Monitor and manage other health conditions: Take steps to manage other health conditions that may increase the risk of dementia, such as diabetes, hypertension, and smoking
Be mindful of early signs: Pay attention to any changes in memory, cognition, or behavior, and seek medical advice if you notice any concerning symptoms. Early detection and intervention can be crucial in managing dementia
Bottom Line:
So, what’s the bottom line? Even though some studies say women might show early signs of dementia more than men, it’s not necessarily the case. That said, there are some gender differences like women being more likely to experience memory difficulties in the early stages of dementia than men. Dementia is a complicated thing, and lots of factors can play a part in whether we get it or not.
I will forever tell everyone I know that there is no harm in seeking functional oversight of your cognition! Find a board-certified medical professional trained in memory, cognition, and neurological-based pathologies to evaluate you. This will allow you to remain in control of your brain health and manage modifiable risk factors.
References
Beam, C. R., Kaneshiro, C., Jang, J. Y., Reynolds, C. A., Pedersen, N. L., & Gatz, M. (2018). Differences Between Women and Men in Incidence Rates of Dementia and Alzheimer’s Disease. J Alzheimers Dis, 64(4), 1077-1083. doi:10.3233/jad-180141
Edahiro, A., Okamura, T., Arai, T., Ikeuchi, T., Ikeda, M., Utsumi, K., . . . Awata, S. (2023). Initial symptoms of early‐onset dementia in Japan: nationwide survey. Psychogeriatrics, 23(3), 422-433. doi:10.1111/psyg.12949
Fitzpatrick, A. L., Kuller, L. H., Lopez, O. L., Diehr, P., O’Meara, E. S., Longstreth, W. T., Jr., & Luchsinger, J. A. (2009). Midlife and late-life obesity and the risk of dementia: cardiovascular health study. Arch Neurol, 66(3), 336-342. doi:10.1001/archneurol.2008.582
Mendez, M. F. (2012). Early-onset Alzheimer’s disease: nonamnestic subtypes and type 2 AD. Arch Med Res, 43(8), 677-685. doi:10.1016/j.arcmed.2012.11.009
Neergaard, J. S., Dragsbæk, K., Hansen, H. B., Henriksen, K., Christiansen, C., & Karsdal, M. A. (2016). Late-Life Risk Factors for All-Cause Dementia and Differential Dementia Diagnoses in Women: A Prospective Cohort Study. Medicine, 95(11). Retrieved from https://journals.lww.com/md-journal/fulltext/2016/03150/late_life_risk_factors_for_all_cause_dementia_and.64.aspx
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K., & Brayne, C. (2014). Potential for primary prevention of Alzheimer’s disease: an analysis of population-based data. Lancet Neurol, 13(8), 788-794. doi:10.1016/s1474-4422(14)70136-x