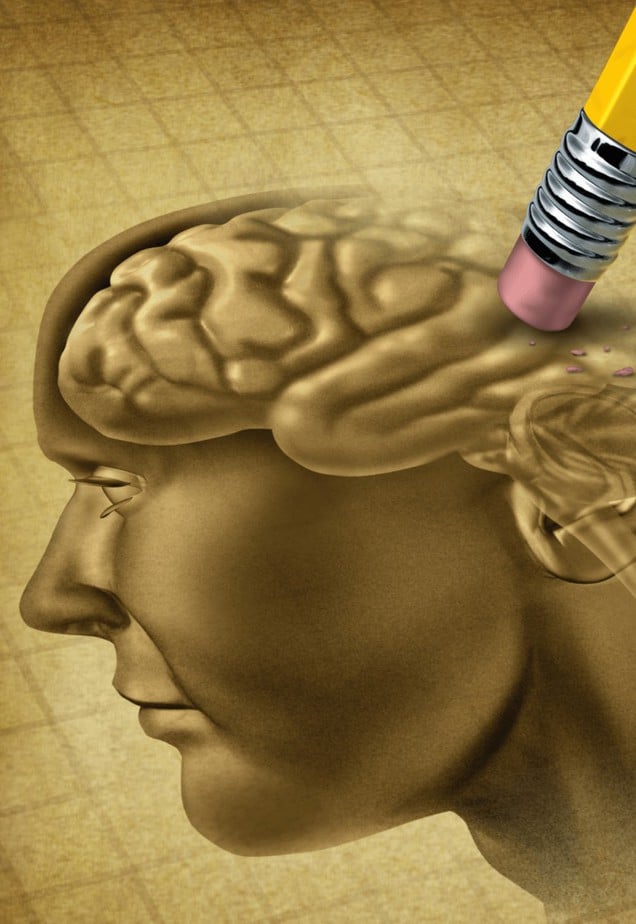
Early Memory Loss and Confusion
Early Memory Loss and Confusion
Authored by Michelle Eliason, MS, OTR/L, CKTS, C.D.S.
If you are experiencing signs and symptoms of early memory loss, it is important to take them seriously. Although there are a variety of factors why you would be having difficulty remembering information, any brain changes should be a concern.
Some symptoms of early memory changes include:
- Word-finding difficulties to items you should know
- Forgetting details of what was said in a conversation or phone call that took place less than 10 minutes ago
- Frequently forgetting why you entered a room (more than 3 times a day)
- Getting lost when driving to locations you have frequently visited
- Personality changes (lethargic, increased desire to be alone, irritable, short-tempered)
- Sleeping more
- Harder time managing finances and appointments
- Increasing difficulty managing tasks you are used to managing (multi-tasking)
- Work performance is being affected at your place of employment
Causes of Early Memory Loss and Confusion
- Stress
- Alcohol and Drugs Misuse
- Anxiety and Depression
- Prescription side-effects
- Neurodegenerative Illness
- Stroke
- Traumatic Brain Injury
- Oxygen Loss
- Brain Infections
Neurodegenerative Illnesses
- Alzheimer’s disease
- Vascular cognitive impairment
- Dementia with Lewy bodies
- Stroke
- Frontotemporal dementia
- Parkinson’s disease
- Huntington’s disease
- Traumatic brain injury
Find out more specific information about your diagnosis:
- Alzheimer’s Disease
- Huntington’s Disease
- Parkinson’s Disease
- Lou Gehrig’s Disease
- Multiple Sclerosis
How can occupational therapy benefit you if you are having early memory loss?
Occupational therapy can greatly benefit you if you are concerned about specific symptoms. Early memory loss is a sign that something somewhere in your brain is not functioning as optimally as it could. Just as you would not ignore your right arm if you were having difficulty raising it, you should not ignore memory loss. With the right early intervention strategies, you can improve your symptoms. You will also have a healthcare professional to monitor your confusion each year in order to provide early intervention if the need arises.
- Comprehensive Evaluation
- Memory screening and follow-up
- Neurocentric Rehabilitation
Occupational Therapy Interventions to Improve Your Memory
What type of intervention is used by a neuro-centered rehabilitation team?
- Neurodevelopmental Techniques
- Proprioceptive Neuromuscular Facilitation
- Cross Crawl Strategies
- Neuromuscular Re-education
- Neurocognitive Strategies
- Heavy Work
- Brain Work
- Habituation Techniques
- Staging
- Screening
- Education
Helpful Page Definititions
Instrumental Activities of Daily Living (IADLs)
Instrumental Activities of Daily Living (IADLs) are essential for independence in life roles and required for aging in place. There are 8 activities core activities for independence including cooking, cleaning, communication, taking and managing medication, handling your personal finances, transportation and community mobility, shopping
Cooking - The ability to follow a recipe and having the stamina to prepare a meal for yourself and/or your family
Cleaning - The ability to perform light housekeeping including making your bed, doing your laundry, washing the dishes, taking out the trash, vacuuming, sweeping, cleaning your bathroom, etc.
Communication - The ability to use the telephone, the computer, have conversations with people (familiar and strangers), communicate your needs clearly.
Taking medication - The ability to sort and organize your medication or determine a compensatory method to do so as well as taking the appropriate dosage at the appropriate time.
Personal Finances - The ability to establish an organization method to understand financial responsibilities and pay your bills on time.
Transportation - Whether you are driving, calling for a driving service like a taxi or Uber, or taking public education. You must have a defined action plan for community mobility and transportation.
Shopping - The ability to plan transportation, plan a grocery/clothing list of needs for yourself and your home, have the stamina to collect your items at the store, and be able to get them into your house.
Activities of Daily Living
Occupational therapists are trained in occupations and activity analysis. An occupation is an activity that you believe is important to your life. There are many levels of occupations, but activities of daily living (ADLs) are the most personal activities and are usually the ones people find most important if they were to lose the ability to complete them.
ADLs include:
- Bathing and showering
- Getting dressed
- Going to the bathroom
- Walking and getting up and down from a chair or car
- Eating and swallowing
- Feeding
- Sexual activity
- Personal hygiene and grooming
- Being able to use personal care devices like adaptive equipment and durable medical equipment
Progressive Neurological Disorders (PND)
Progressive Neurological Disorders (PNDs) are diagnoses that are progressive in nature and cause a decline in function throughout their progression. They are also known as neurodegenerative diseases. The decline can be seen over decades, years, months, or even weeks.
Some common examples of PNDs include Multiple Sclerosis, Parkinson's disease, Lewy Body Dementia, Lou Gerhig's Disease, Alzheimer's disease, Motor Neuron Disease, and Huntington's disease.
Early intervention for any neurodegenerative disease is critical to maintaining function for as long as possible. Restoration in early stages and maintenance throughout a disease progression can benefit your quality of life and reduce caregiver burden.
Neuromuscular Re-education
NMRE is used by neurocentric occupational therapists to improve communication between your muscular system and nervous system. By promoting this stream of communication, you close the circle of recovery. Without NMRE, you can have the biggest muscles in the world and still experience mobility deficits due to poor reaction time, coordination, and mixed signals.
Heavy Work
Heavy work is also known as resistance training and can utilize isometric and isotonic movements with or without external weights while focusing on eccentric and concentric muscle contractions. By partnering heavy work with visual perceptual tasks and neural recruitment visualization, increased carryover and recovery is experienced.
Neurodevelopmental Techniques (NDT)
NDT is a hands-on approach used by occupational therapists to provide deep pressure to key parts of your body during repeated movements. Your movement mixed with repetition and deep pressure creates and stores new motor patterns in your brain in order to re-establish mobility and speed up recovery.
Proprioceptive Neuromuscular Facilitation (PNF)
NDT is a hands-on approach used by occupational therapists to provide deep pressure to key parts of your body during repeated movements. Your movement mixed with repetition and deep pressure creates and stores new motor patterns in your brain in order to re-establish mobility and speed up recovery.
Cross Crawl Techniques
A cross-crawl technique is used in movement and mobility training of both upper body and lower body. By recruiting both sides of your brain using opposite movement patterns we strengthen the communication across the two sides of your brain known as your corpus collosum.
Neurocognitive Strategies
When combining neurcogitive skills and functions with motor elements, true cognitive rehabiliation can take place (memory, recall, sequencing, etc.). We include the domains of neurocognition like language, calculation, executive functioning, complex attention, perceptual-motor, and reasoning while training your body in order to increase neural plasticity and neural re-patterning.
Comprehensive Evaluation
Occupational therapists treat the entire person. Much like your primary care physician, we were required to learn elements of the entire body so that we could treat holistically (a one stop shop). Because of this, your outpatient rehabilitation specialist will perform an evaluation that assesses the following things:
- Personal history
- Who are you? What do you do? What makes you tick? Why are you seeking outpatient therapy?
- Physical function (upper body and lower body)
- Strength, range of motion, and flexibility
- Neuromuscular function (brain to muscle communication)
- Coordination, speed, agility, and reaction time
- Cognitive and Mind health
- Short term memory, recall, information processing, and perception of illness
- Occupational Inventory (Activity and role inventory)
- Roles you play like a caregiver, spouse, parent, employee, etc.
- Mobility inventory like the places you need to go
- IADL inventory and what activities are required for you to be independent
- Other activities that are important to you