Balance Activities for Occupational Therapy Interventions
General:
Balance Activities in occupational therapy services are unique in that the OTP is thinking about the occupational performance, future multi-context implications, and (most importantly) the source of the client’s dysfunction so that it can be remediated or restored to it’s maximum capacity. An occupational therapy practitioner should never forget that our primary role is to restore function the correct way in order to allow our client to live a least-restrictive lifestyle. We must apply the study of medicine to analyze our client’s diagnosis, the study of biomechanics and kinesiology to restore and maximize function, and the psychosocial model in order to provide a balance between the medical and social science frame of mind. THIS is occupational therapy!
Assessments to use in Evaluation and Progress Notes:
- BERG Balance Assessment
- Timed Up and Go
- 5 Times Sit to Stand
- 10ft Tandem Line
- Modified Falls Efficacy Scale
- ABC Balance Scale
Balance and Stability Course
Learn core structures from an OT Practitioner who works with these structures every day! Have a better understanding of structural anatomy and how to apply this information directly to your treatments!
What you’ll get:
- Over three hours of recorded training
- 15 Handouts and Tip Sheets from the BOT Resource Portal
- More confidence to incorporate therapeutic exercise and neuromuscular re-education into your OT clinical practice
As occupational therapists, navigating the intricacies of reimbursement and avoiding duplicate services can be challenging. Whether you’re working in skilled nursing facilities (SNFs), assisted living facilities (ALFs), or outpatient settings, precise documentation and goal-setting are essential. Here’s a guide to help you understand the importance of effective documentation and how to enhance your practice, particularly when addressing balance and stability.
The Importance of Documentation
Effective documentation is the cornerstone of occupational therapy practice. It ensures that your interventions are recognized, reimbursed, and aligned with your patient’s goals. The way you document and write your goals reflects your approach as an occupational therapy practitioner. Detailed and accurate documentation not only supports reimbursement but also distinguishes your role from other healthcare providers, such as physical therapists (PTs).
Addressing Duplicate Services
A common concern among occupational therapists is the issue of duplicate services. This often arises when multiple therapists, such as PTs, are working on similar goals like improving balance for ambulation or transfers. However, it’s essential to understand that you can still bill for these functions by emphasizing your unique occupational therapy perspective. The key lies in the language you use and the details you provide in your documentation.
Leveraging SMART Goals
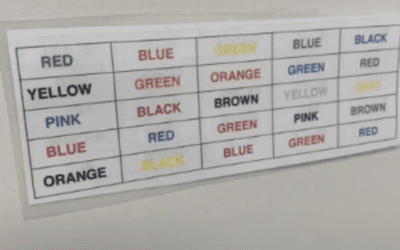
One effective strategy is to use SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound. On the BOT portal, there is a training course on SMART goals that is part of the Connect Mentorship Program. This course provides valuable insights into setting clear and actionable goals. Additionally, I’m updating the documentation examples with a color-coding system to highlight where and why occupational therapy fits into the remediation process. This approach helps in clearly defining your interventions and linking them to occupational outcomes.
Understanding Balance and Stability
When working on balance and stability, it’s crucial to differentiate between these two concepts. Balance involves maintaining equilibrium without movement, often requiring proprioception and postural control. Stability, on the other hand, involves using balance during movement and engaging in multi-activity occupations within context. Knowing these differences allows you to tailor your interventions more effectively.
For instance, if PTs are working on ambulation and transfers, focus on other aspects of balance and stability that support these functions. Use sensory enhancement, strength training, or proprioceptive exercises to address specific deficits. Document these interventions thoroughly, using OTPF language and linking them to occupational goals. This approach not only ensures reimbursement but also highlights the unique value of occupational therapy.
Defensive Documentation
Defensive documentation is another critical aspect. Always be prepared to justify your interventions with clear rationales. Use specific OTPF language and patient assessments, such as the ABC Confidence Scale or the Modified Falls Efficacy Scale, to support your documentation. This practice not only protects you from audits but also reinforces the breadth of your practice.
Utilizing Resources
Take advantage of available resources like the Connect Mentorship Program and the color-coded documentation system. These tools are designed to enhance your practice by providing comprehensive knowledge and practical strategies for effective documentation. Engaging with your professional network and participating in mentorship programs can also build your confidence and improve your practice.