Understanding the Difference: Therapeutic Exercise, Therapeutic Activity, and Neuromuscular Re-education in Occupational Therapy
Understanding the Difference between Therapeutic Exercise and Neuromuscular Re-Education in Occupational Therapy
As dedicated professionals in the field of occupational therapy, we are constantly striving to provide the best possible care for our clients. One crucial aspect of our practice is understanding the nuances between different treatment modalities and knowing when to apply each one effectively. It is important to know the distinctions between three commonly used billing codes: Therapeutic Exercise (97110), Therapeutic Activity (97530), and Neuromuscular Re-education (97112), with a focus on their relevance in adult populations.
Therapeutic Exercise (97110)
Therapeutic Exercise (97110): This billing code is utilized when engaging in interventions aimed at addressing specific joints, structures, or muscles. In alignment with the Biomechanical model of practice, therapeutic exercises are designed to remediate, restore, or maintain the integrity of these elements. Examples of treatments may include:
- Strengthening exercises for individuals recovering from orthopedic surgeries such as total knee replacements.
- Range of motion exercises for patients with rheumatoid arthritis to maintain joint mobility and prevent contractures.
- Endurance training for individuals with chronic obstructive pulmonary disease (COPD) to improve tolerance for daily activities.
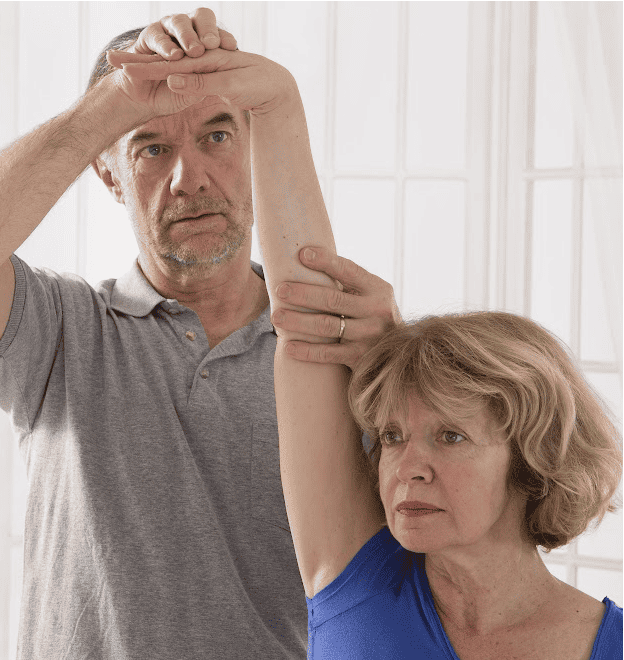
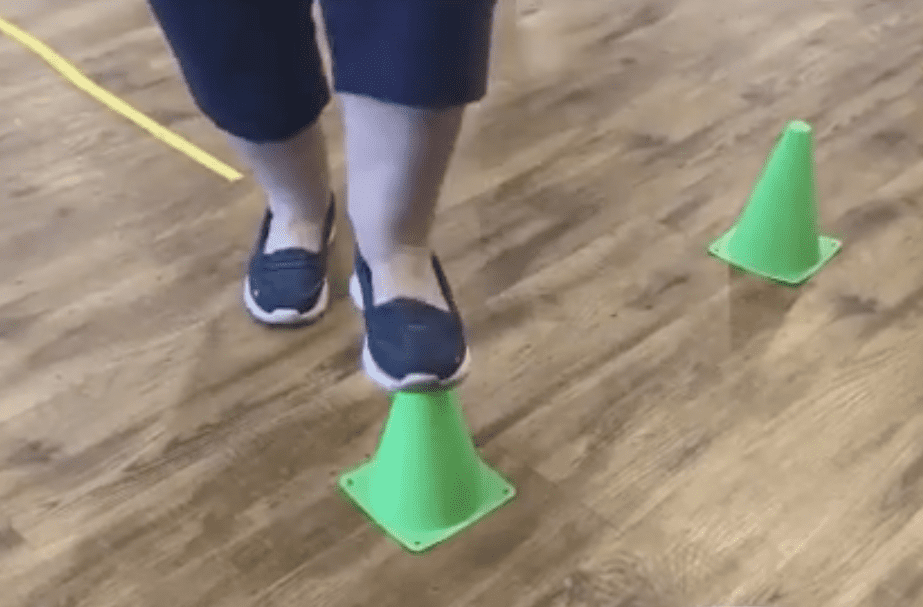
Neuromuscular Re-Education (97112)
Neuromuscular Re-education (97112): Contrary to common belief, Neuromuscular Re-education (NMRE) does not exclusively pertain to neurological-based diagnoses. Instead, it encompasses various neurological models of practice within the occupational therapy scope. NMRE interventions target balance, coordination, kinesthetic sense, posture, and proprioception for sitting and/or standing activities. Examples may include:
- Core stabilization exercises for individuals with low back pain to improve posture and prevent further injury.
- Dual-tasking exercises for older adults at risk of falls to improve cognitive-motor integration and balance control.
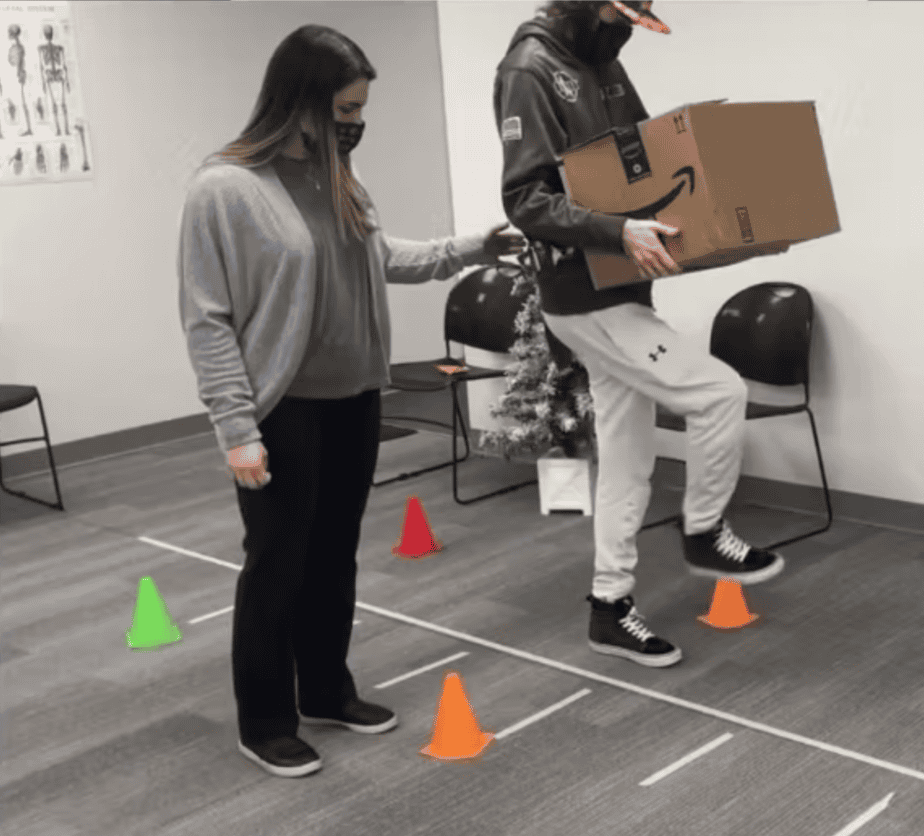
Therapeutic Activities (97530)
Therapeutic Activity (97530): Therapeutic activities are movement-based interventions that occur outside of the personal context of the client but often simulate real-life tasks. These activities are designed to improve functional performance and are billed under the therapeutic activity code (97530). Examples include:
- Simulated work tasks such as sorting objects or assembly tasks for individuals undergoing vocational rehabilitation.
- Community mobility exercises such as navigating public transportation or crossing streets safely for clients with mobility impairments.
- Environmental adaptations tasks such as practicing using adaptive equipment or modifying home environments for individuals with physical disabilities.
- Core stabilization exercises for individuals with low back pain to improve posture and prevent further injury.
- Dual-tasking exercises for older adults at risk of falls to improve cognitive-motor integration and balance control.
Bottom Line:
Understanding the distinctions between Therapeutic Exercise, Therapeutic Activity, and Neuromuscular Re-education is essential for providing comprehensive and effective care in occupational therapy practice. By selecting the appropriate billing code and tailoring interventions to the individual needs and goals of our clients, we can maximize outcomes and promote optimal function and participation in daily life.