Traumatic Brain Injury Rehabilitation TBI
Traumatic Brain Injury (TBI) Rehabilitation and Support Services

What is a Traumatic Brain Injury (TBI)
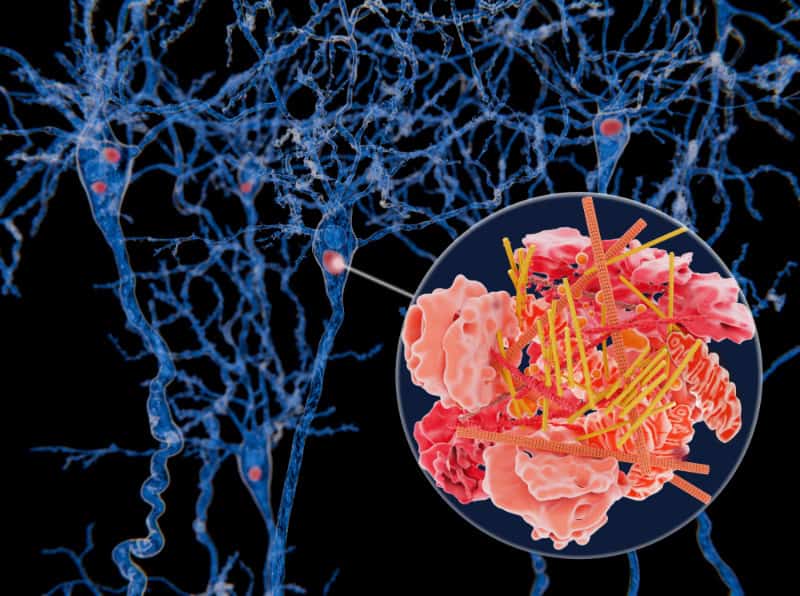
A traumatic brain injury (TBI) can occur after a fall, sport injury, motor vehicle accident, blunt force trauma, accident at work, or any other occurrence causing the brain to be jolted or damaged in some way. The severity of the injury can range from mild to severe, and you may experience symptoms lasting days, weeks, months, or even years.
Most people will begin the recovery process of a TBI in an inpatient hospitalization setting where you will regain physical, sensory, behavioral, and cognitive function. If you experienced a TBI resulting in concussion, but is not so severe that you require inpatient hospitalization, you should be immediately beginning community-based outpatient occupational therapy. In a more severe case, outpatient occupational therapy will be part of the continuum of care. Making sure you see a therapy team familiar with the symptoms and recovery process of a traumatic brain injury is crucial to maximizing your outcomes.
Symptoms of
Traumatic Brain Injury (TBI)
Physical Symptoms
- Headaches and migraines
- Impaired balance and dizziness
- Neck and lower back pain
- Upper body and lower body muscle weakness
- Loss of coordination
- Difficulty sleeping and staying asleep
Emotional Symptoms
- Mood changes
- Personality changes
- Increase volatility and short-tempered
- Unable to balance emotions
- Increased desire to be alone
Cognitive Symptoms
- Confusion
- Decreased executive functioning
- Short attention span
- Short term memory deficits
- Impaired information processing speed
- Impaired multi-tasking ability
- Impaired working memory skills
- Word finding difficulties
Sensory Symptoms
- Tremors in hands, legs, or feet
- Neuropathy, paresthesia, numbness, or tingling in hands and feet
- Depth perception difficulties
- Visual perceptual deficits
- Sensitivity to light and sound
- Ringing in your ears (tinnitus)
- Taste changes or lack of appetite
For more information, check out the Brain Injury Association
Meaningful Activities (Occupations) affected by a Traumatic Brain Injury (TBI)
- Bed mobility
- Cleanliness and thoroughness while toileting
- Showering and maintaining safety
- Dressing
- Mobility (standing tolerance, walking, getting up and down without dizziness)
- Driving
- Caring for children or loved ones
- Housekeeping
- Working or remaining at work (vocational rehabilitation)
- Managing medications, finances, and appointments
Other Occupations (meaningful activities)
- Maintaining volunteer roles
- Participating in hobbies or extra-curricular activities
- Going to church
- Exercising
Why is outpatient occupational therapy imperative for Traumatic Brain Injury
- Outpatient occupational therapy can help you long-term and address your full recovery after a stroke
- upper body and lower body physical function
- Tremors
- Neuropathy and paresthesias
- Mobility
- Balance
- Cognitive function
- Safety awareness and sequencing
- Instrumental Activities of Daily Living
- Activities of Daily Living
- Outpatient occupational therapy can see you as needed and maintains an occupational profile to ensure we stay current on your long term stroke recovery process.
- Occupational therapy addresses the entire person with an emphasis on your physical body and performance skills, the environment or physical space you find yourself in, and the types of activities that have been affected by your stroke.
What are some problems an occupational therapy can help solve?
- Your ability to move (upper and lower body mobility)
- Range of motion including effects of a joint contracture, spasticity, or flaccidity
- Your ability to take care of your own personal care (ADLs)
- Your ability to complete essential activities for independence (IADLs)
- Learning techniques to improve your planning, reasoning, and organization
- Getting into and out of your home
- Working and returning to work
- Wheelchair Assessments and Positioning
- Community Mobility
- Remaining independent in your home
- Addressing personal concerns, worries, and psychosocial barriers that may be preventing rehabilitation progress
References
Altman, I. M., Swick, S., Parrot, D., & Malec, J. F. (2010). Effectiveness of community-based rehabilitation after traumatic brain injury for 489 program completers compared with those precipitously discharged. Archives of Physical Medicine and Rehabilitation, 91, 1697–1704.
Kim, H., & Colantonio, A. (2010). Effectiveness of rehabilitation in enhancing community integration after acute traumatic brain injury: a systematic review. American Journal of Occupational Therapy, 64, 709–719. https://dx.doi.org/10.5014/ajot.2010.09188
Traumatic brain injury. (2019, March 29). Retrieved March 13, 2020, from https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
Traumatic brain injury. (2019, March 29). Retrieved March 13, 2020, from https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557