Lewy Body Dementia and Rehabilitation
Lewy Body Dementia
Lewy Body Dementia is a condition that looks different for each person, but the way the disease works in the brain, known as pathogenesis, follows the same general pattern. Some specialized physical, occupational, and speech therapists are trained in understanding how the disease spreads through the brain and how it impacts different functions over time. These changes are specific to Lewy Body Dementia, making your journey with LBD different from someone with Alzheimer’s, frontotemporal dementia, or Parkinson’s.
If you’ve been diagnosed with LBD, it’s important to start building your long-term management team. While you won’t need therapy or medical appointments all the time, you will benefit from having periods of therapy when changes in your body or function start to appear. Having someone to contact when these changes happen ensures you can get the right support at the right time. Early diagnosis and intervention are key to maintaining as much independence and function as possible throughout the course of the disease.
What is Lewy Body Dementia?
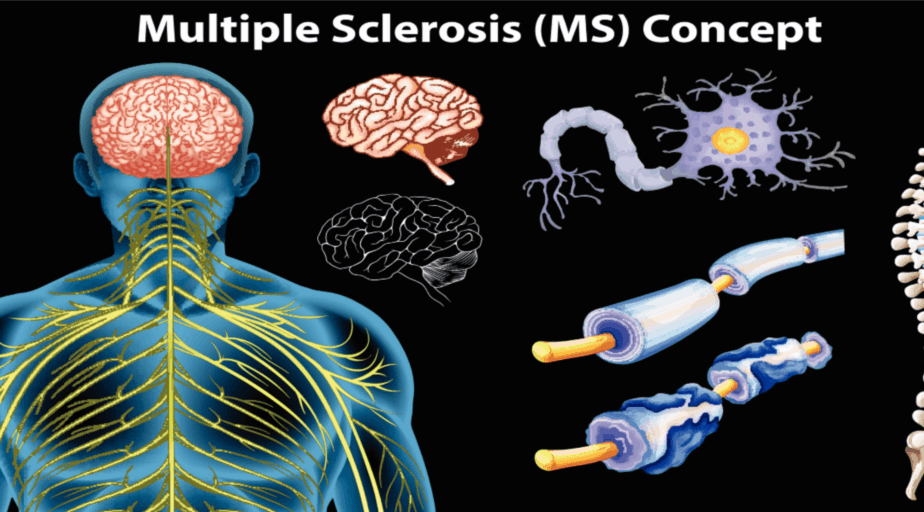
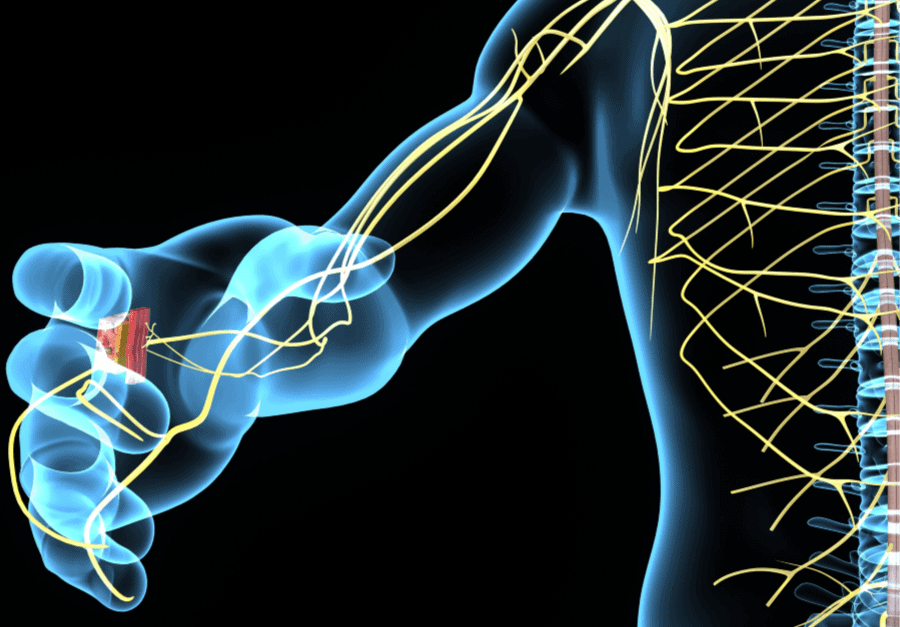
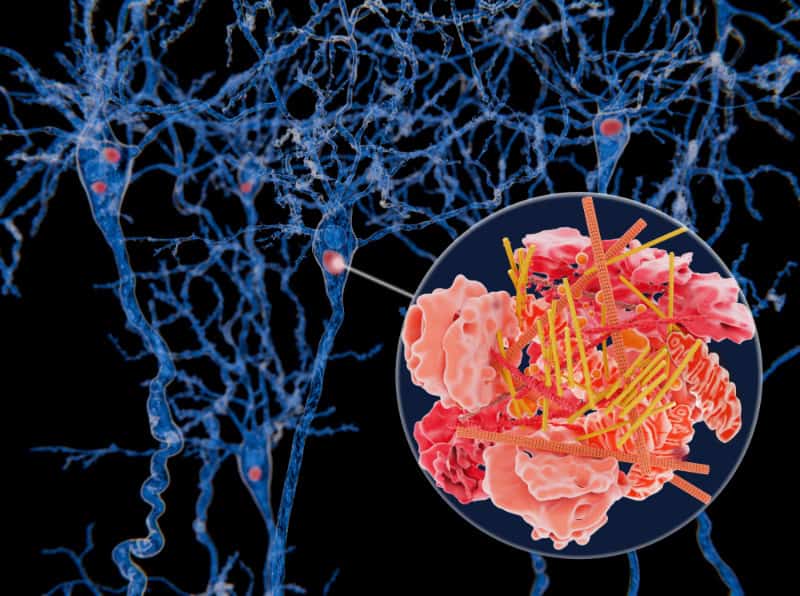
Lewy Body Dementia (LBD) is the second most prevalent progressive neurodegenerative diagnosis causing dementia. It is second to Alzheimer’s disease (AD), but differs in many ways. It is signified by lewy body proteins that appear in various parts of your brain affecting thinking, functional activities, judgement, executive function, functions of the autonomic nervous system, and mobility.
The Lewy Body Association has more information regarding the difference between Alzheimer’s Disease (AD) and Lewy Body Disease (LBD).
What do I do if I’ve been diagnosed with Lewy Body Dementia (LBD)?
After receiving an LBD diagnosis, it is important to establish a long-term therapy team including occupational therapy, speech therapy, and physical therapy familiar with the progression of this diagnosis. By establishing a small therapy team that will be able to remain with you throughout the stages of Lewy Body Dementia, you will be able to maximize your physical function, maintain your performance in functional activities, and ensure you remain in control of your symptoms instead of the other way around.
Symptoms of Lewy Body Dementia
- Runny Nose
- Visual hallucinations (detailed)
- Delusions
- Agitation and frustration
- Difficulty multi-tasking or remaining on task
- Information processing difficulties
- Stooped posture (similar to Parkinson’s disease)
- Overall movements and mobility slowing down
- Balance and coordination decline
- Walking turns into a ‘shuffle’
- Voice becomes more quiet
For more symptoms of Lewy Body Dementia, head to Alzheimer’s Association.
What are my options after receiving an LBD diagnosis?
Although there are neurocognitive enhancement medications, one of the most important things you can do for yourself is to seek out a team of therapists as early as possible. With the right early intervention strategies you can improve your symptoms and/or control the speed at which you experience decline.
What type of intervention is used by a neuro-centered rehabilitation team?
- Neurodevelopmental Techniques
- Proprioceptive Neuromuscular Facilitation
- Cross Crawl Strategies
- Neuromuscular Re-education
- Neurocognitive Strategies
- Heavy Work
- Brain Work
- Habituation Techniques
- Functional training to ensure you can remain independent in self-care (ADLs) and other activities of independence (IADLs) for as long as possible
- Staging
- Screening
- Education
How can outpatient occupational therapy help after a dementia diagnosis?
- Once given a dementia diagnosis, we can ‘stage’ your dementia progression through specific screens and assessments so that you always feel in control of your circumstances.
- Make recommendations for adaptive equipment, durable medical equipment, and mobility aids throughout each stage
- Provide a hybrid approach to rehabilitation and maintenance grounded in neurocentric principles offering you an inclusive rehab program.