Warning Signs of Dementia
“Memory is the diary that we all carry about with us.” – Oscar Wilde
Warning Signs of Dementia
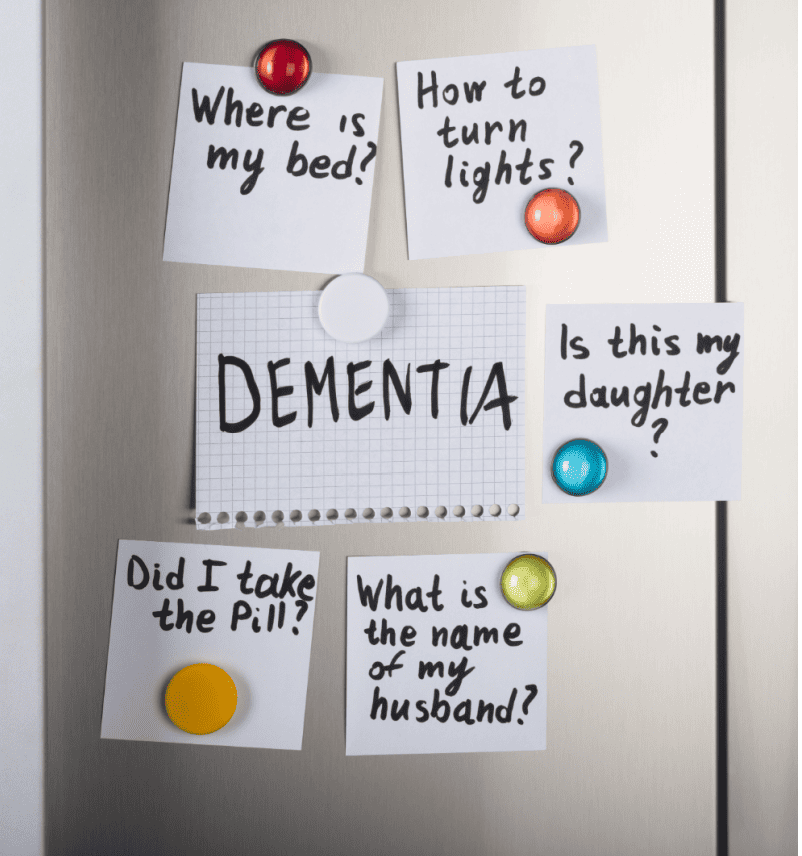
Memory changes as we age can be unsettling, leaving many of us wondering if what we’re experiencing is just a normal part of getting older or something more serious, like dementia. It’s important to recognize that there’s a subtle overlap between age-related memory changes and the warning signs of dementia. In this article, we’ll explore these warning signs in a way that’s easy to understand.
Consider the following symptoms of Dementia:

Working Memory
Working Memory
Do you find it challenging to remember things you just learned or heard? This could be a sign of dementia.

Episodic Memory
Episodic Memory
Trouble remembering specific events or experiences from your past.

Immediate Recall Difficulty
Immediate Recall Difficulty
Struggling to remember information right after learning it.

Slower Retrieval and Rapid Forgetting
Slower Retrieval and Rapid Forgetting
Finding it takes longer to recall information, and forgetting things more quickly.

Prospective Memory Challenges
Prospective Memory Challenges
Difficulty remembering to perform tasks in the future without external reminders.

Autobiographical Memory Changes
Autobiographical Memory Changes
Memories across your lifespan become less detailed and more vague.
What can ‘offset’ these changes or help you cope with them?
Intelligence, expertise, and using compensatory strategies can help cope with memory changes.
Examples:
- Using tools like calendars or setting reminders on your phone to help remember important dates or tasks.
- Using mnemonic devices to remember important information.
- Writing notes to yourself to remember tasks or appointments.
- Creating a daily routine to help remember daily tasks and activities
Note: Memory specialists are trained with information that greatly exceeds these very simple everyday strategies found on the internet. Clinical oversight is recommended if you feel some of these symptoms have described you.
Bottom Line:
If you or a loved one are experiencing these warning signs of dementia, it’s essential to seek help from a local memory specialist. While it can be challenging to confront these changes, getting an evaluation and discussing options early on can lead to better outcomes and quality of life. Remember, you’re not alone, and there are resources available to support you through this journey.
References
Baddeley, A. D., Kopelman, M. D., & Wilson, B. A. (2004). The essential handbook of memory disorders for clinicians. Chichester, West Sussex, England ;: J. Wiley.
Cohen, C., Culver, C., Gomberg, D., Magai, C., & Malatesta, C. (1996). Emotional Expression During Mid- to Late-Stage Dementia. International psychogeriatrics, 8(3), 383-395. doi:10.1017/S104161029600275X